What is Neuropathy?
What is Neuropathy?
Neuropathy, often called peripheral neuropathy, is a condition in which one or more nerves are damaged or dysfunctional. There are three different forms of neuropathy, namely mononeuropathy, multiple mononeuropathies or mononeuropathy multiplex, and polyneuropathy. When only one nerve is affected, it is called mononeuropathy. When two or more nerves are affected, it is called multiple mononeuropathies or mononeuropathy multiplex. When many or most peripheral nerves are affected, it is called polyneuropathy. Regardless of form, neuropathy typically starts in the hands and feet, though other body parts can be affected as well.
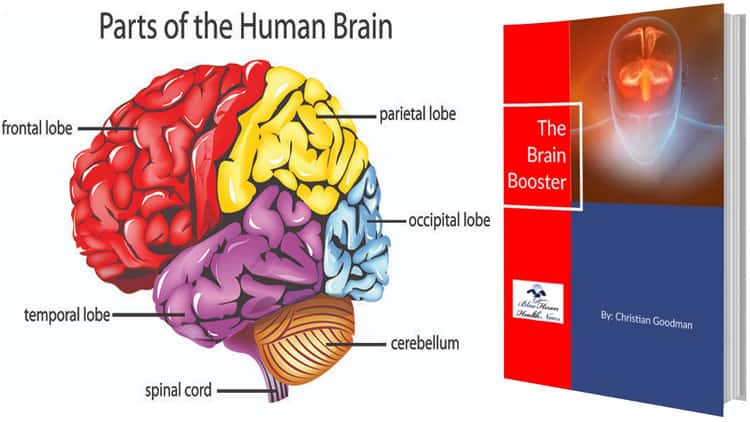
The peripheral nervous system, or PNS, encompasses the nerves that lie outside the brain and spinal cord. Within the PNS, there are three types of nerves – sensory nerves, motor nerves, and autonomic nerves. Each type is responsible for a different set of tasks, which work together to keep the body functioning as it should. Sensory nerves carry sensory information to the central nervous system, motor nerves send motor signals to the muscles which control muscle movement, and autonomic nerves control functions such as the bladder, heart rate, digestion, and blood pressure. When the nerve signal transmission to any of these nerves is disrupted, neuropathy can occur.
The leading cause of neuropathy is diabetes, a condition known as diabetic polyneuropathy. This is because high blood sugar levels as a result of either type 1 or type 2 diabetes can lead to nerve damage. Other causes of peripheral neuropathy include a viral infection, physical injury to the nerves, and a side effect of excessive alcohol or certain medicines. As for common symptoms of neuropathy, these include a shooting pain in the affected area, loss of balance and coordination, tingling and numbness in the hands or feet, and muscle weakness. Symptoms of neuropathy are most often constant, but may also come and go in waves.
In order to diagnose a patient with neuropathy, doctors may order blood tests, ask about symptoms, and examine the affected area. Blood tests can check for vitamin B12 deficiency and diabetes, while physical examinations may involve testing strength, reflexes, and sensations. In some instances, individuals may be sent to a neurologist for a nerve conduction study and electromyography. A nerve conduction study, or NCS, measures the strength and speed of the nerve signal with electrodes. These small metal wires are placed on the skin and stimulate the nerves by releasing small electric shocks. Electromyography, or EMG, measures the electrical activity of the muscles by inserting a needle through the skin.
Possible complications of peripheral neuropathy depend on the cause and the nerves that are damaged. For example, a foot ulcer that becomes infected can cause gangrene, a serious condition in which a lack of blood supply leads to tissue death. Similarly, treatment for neuropathy depends on the underlying causes as well as the symptoms. For instance, sufferers who experience muscle weakness may receive treatment in the form of walking aids and physical therapy. Those who experience nerve pain may be prescribed neuropathic pain agents since standard painkillers typically don’t work. People with diabetes may be told to limit alcohol and stop smoking, in addition to gaining control of their blood sugar levels.
Causes and Risk Factors of Neuropathy
The leading cause of neuropathy in both the United States and the United Kingdom is diabetes. In fact, between 60% and 70% of patients with diabetes will experience some degree of damage to their nerves. In addition to diabetes, there are a number of other health conditions that can lead to peripheral neuropathy. Namely autoimmune diseases, infections, inherited disorders, tumors, bone marrow disorders, and various other diseases. Beyond health conditions, other causes include certain medications, exposure to toxic substances, alcoholism, vitamin deficiencies, and trauma that puts pressure on the nerves. In contrast, idiopathic neuropathy is a condition in which no known cause can be identified. This is a somewhat common condition that occurs in individuals above the age of 60.
Autoimmune diseases that are known to cause peripheral neuropathy include rheumatoid arthritis, Sjogren’s syndrome, chronic inflammatory demyelinating polyneuropathy, Guillain-Barre syndrome, lupus, and vasculitis. Rheumatoid arthritis is a long-term inflammatory disorder that affects the joints, Sjogren’s syndrome is a condition in which the immune system accidentally attacks the glands responsible for making tears and saliva, and CIDP is a neurological disorder that involves inflammation of peripheral nerves and destruction of the myelin sheath. Moreover, Guillain-Barre syndrome is a rare disorder in which the immune system attacks the nerves, lupus is a condition in which the immune system attacks healthy tissue, and vasculitis refers to a group of disorders involving inflammation of the blood vessels.
Signs and Symptoms of Neuropathy
Neuropathy can affect sensory nerves, motor nerves, and autonomic nerves. Since different nerves have different functions, symptoms typically vary based on the type of nerves that are affected. Sensory nerves, also called afferent nerves, carry sensory information to the central nervous system. The sensory information that these nerves receive includes pain, temperature, touch, and vibration from the skin. Motor nerves are located in the central nervous system and send motor signals to the muscles, thereby controlling muscle movement. Autonomic nerves belong to the autonomic nervous system and control functions such as the bladder, heart rate, digestion, and blood pressure.
Peripheral neuropathy can affect one nerve, two or more nerves, or many nerves. These conditions are referred to as mononeuropathy, multiple mononeuropathy, and polyneuropathy, respectively. The most common type of peripheral neuropathy is polyneuropathy, while the most common form of mononeuropathy is carpal tunnel syndrome. This is a condition in which the median nerve in the wrist becomes compressed, leading to pain, tingling, or numbness in the fingers. Other types of mononeuropathy may lead to weakness on one side of the face, problems with focusing the eyes, and foot or shin pain. In terms of symptom development, neuropathy can either be acute or chronic. Acute neuropathy means that symptoms appear suddenly, whereas chronic neuropathy means that symptoms develop slowly over time.
When sensory nerves are involved, signs and symptoms may include loss of balance and coordination, pins and needles in the affected body part, increased sensitivity to touch, decreased ability to feel pain or temperature changes, sharp pains or cramps in the body, a tingling or burning sensation around the affected area, and various foot problems – from bone pain and ulcers to infections and joint pain. These signs and symptoms typically start in the feet and legs, then move to the hands and arms, and are generally worse at night.
When motor nerves are involved, the main symptom is muscle weakness or paralysis, which can affect one muscle or several muscles. Paralysis is a temporary or permanent condition, depending on the cause, and refers to the inability to move a part of the body or the entire body. Additional signs and symptoms include muscle atrophy, twitching, foot drop, painful cramps, and fasciculations. Muscle atrophy refers to muscle shrinking or muscle wasting, caused by the inability to move a certain body part. Foot drop refers to difficulty lifting the front part of the toes and feet, while fasciculation refers to uncontrolled muscle twitching.
Stages of Neuropathy
Peripheral neuropathy often occurs in five stages, starting with sporadic pain and numbness during stage one, and ending with a complete loss of feeling in the feet and lower legs by stage five. The in-between stages are characterized by more frequent pain in stage two, pain that reaches its peak during stage three, followed by constant numbness of the affected areas throughout stage four. The different stages of neuropathy are not always easy to recognize, which is why it’s important to understand how the condition progresses in order to take the right measures to prevent the continuation of this debilitating condition.
Stage one of neuropathy is characterized by sporadic pain and numbness. Symptoms are generally mild and subtle and are most often caused by excessive sugar consumption. It is therefore recommended that you make some dietary adjustments, like cutting back on junk food, carbohydrates, and sweets. During this first stage, the pain and numbness tend to come and go. Additional symptoms include loss of balance and poor reflexes, though this is typically minor so there is no cause for concern. Some may go weeks or even months between experiencing symptoms.
Stage two of neuropathy is characterized by more frequent pain and more regular symptoms than in stage one. The pain is more severe and the numbness is more consistent, making it harder to ignore these symptoms. Most sufferers will book an appointment with a doctor at some point during this stage since the pain is now extreme enough for them to know that something is wrong. This is a very important stage of neuropathy, since it is considered to be the last chance to treat whatever underlying condition is causing the neuropathy before the nerve damage becomes permanent.